Chronic Illness, Misdiagnosis & the Truth About Tick-Borne Disease: Dr. Susan Marra on Doctors Making a Difference Podcast
In a recent episode of the podcast Doctors Making a Difference, Dr. Susan Marra joins host Dr. Steven Crane to discuss one of today’s most misunderstood and frequently misdiagnosed health challenges: chronic tick-borne disease.
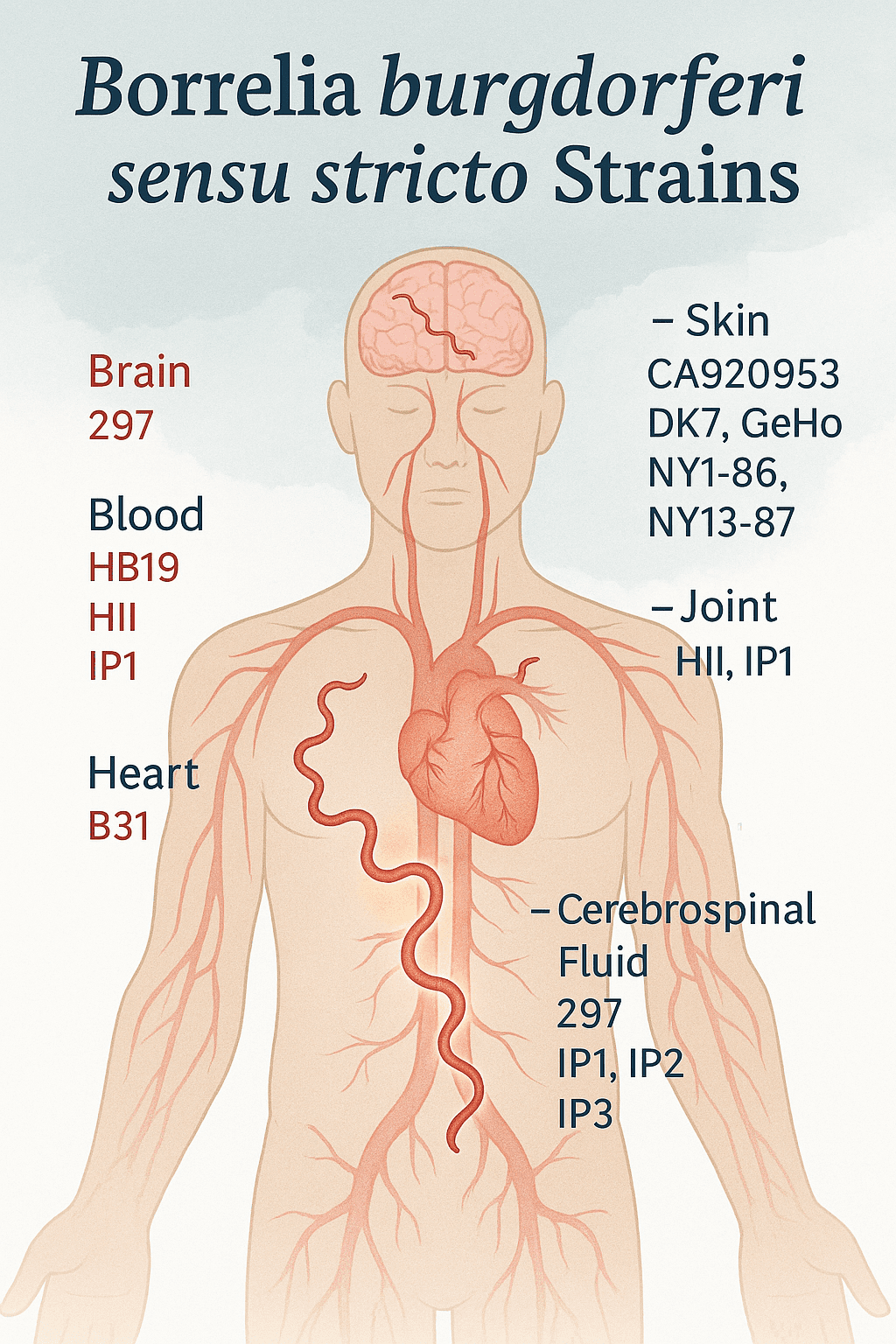
In the episode “Chronic Illness, Misdiagnosis & the Truth About Tick-Borne Disease with Dr. Susan Marra,” she explains why many patients with unusual, multisystem symptoms are actually living with chronic Lyme disease, Bartonella, Babesia, and other co-infections, and why standard testing often misses the majority of cases.
Below is the full video interview, key insights, and a complete timestamp guide for quick navigation.
Watch the Full Episode:
Other Ways to Listen
About the Episode
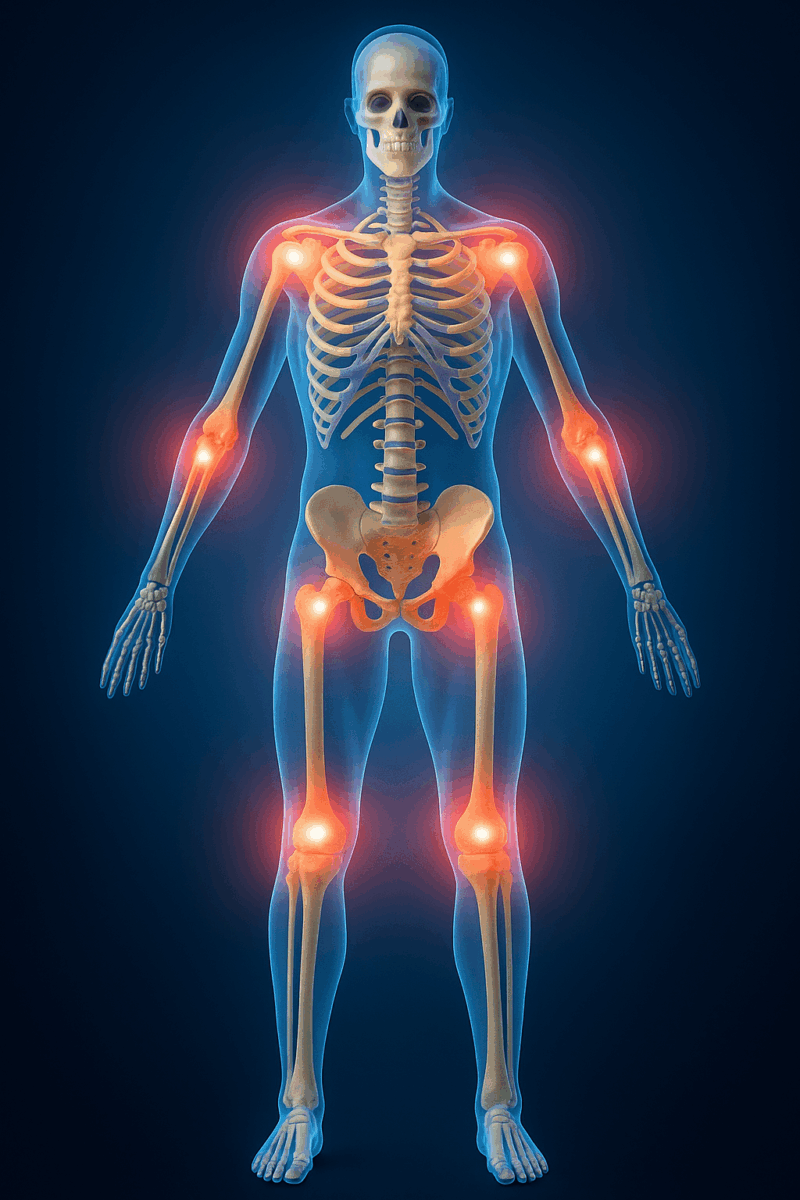
Many patients spend years searching for answers to symptoms like migratory pain, neurological issues, chronic fatigue, gastrointestinal problems, and cognitive decline.
In this conversation, Dr. Marra breaks down:
- Why these symptoms often point to tick-borne illness
- How co-infections complicate diagnosis and treatment
- Why standard testing fails to detect most cases
- What emerging diagnostics and research are revealing
- How physicians can better recognize and support these patients
Timestamps
00:00 — Welcome to Doctors Making a Difference
01:01 — Meet Dr. Susan Marra: Psychology background & early career
02:55 — Discovering a Wave of Strange Symptoms
04:02 — The First Clues: Migratory Pain, Brain Fog, GI Issues
05:45 — Connecting with Early Lyme Experts
07:02 — Dr. Marra Gets Lyme Herself
08:14 — Losing Vision and the Road to Recovery
10:01 — Why Standard Lyme Tests Fail
11:40 — Understanding Co-Infections: Babesia, Bartonella & More
13:21 — Modern Diagnostics: PCR, FISH & Specialty Labs
15:00 — Why Insurance Often Won’t Cover Testing
16:42 — The Cost Barrier in Tick-Borne Illness
18:03 — Why “Just Lyme” Rarely Exists Anymore
19:25 — Navigating Controversy in Tick-Borne Medicine
21:14 — How Patients Find Her Expertise
23:03 — Advances in Treatment Over 27 Years
24:55 — Methylene Blue, Dapsone & Emerging Therapies
26:30 — Botanical Medicine vs. Antibiotics
28:18 — How Tick-Borne Illness Alters Genetics & Immunity
30:02 — Research: Hygromycin A, Dapsone Trials & More
32:01 — The Biggest Concerns: Transfusion & Congenital Transmission
34:12 — What Physicians Must Recognize in Their Patients
36:20 — How to Assess Risk & Choose the Right Tests
38:00 — Dr. Marra’s Website & Resources for Physicians
39:20 — Closing Thoughts from Dr. Crane
About Dr. Susan Marra
Dr. Susan Marra is an award-winning clinician with over 27 years of experience in diagnosing and treating complex, chronic illnesses, including Lyme disease, Bartonella, Babesia, mold illness, and other immune-disrupting infections. Her personal experience with Lyme disease shapes her compassionate, evidence-informed approach to patient care.
About the Podcast: Doctors Making a Difference
Hosted by Dr. Steven Crane, Doctors Making a Difference is a podcast highlighting physicians and researchers who challenge conventional assumptions, push medicine forward, and advocate for patients who often fall through the cracks.