Understanding Fibromyalgia (FM)
Fibromyalgia (FM)
Understanding the Underlying Causes of Widespread Pain and Fatigue
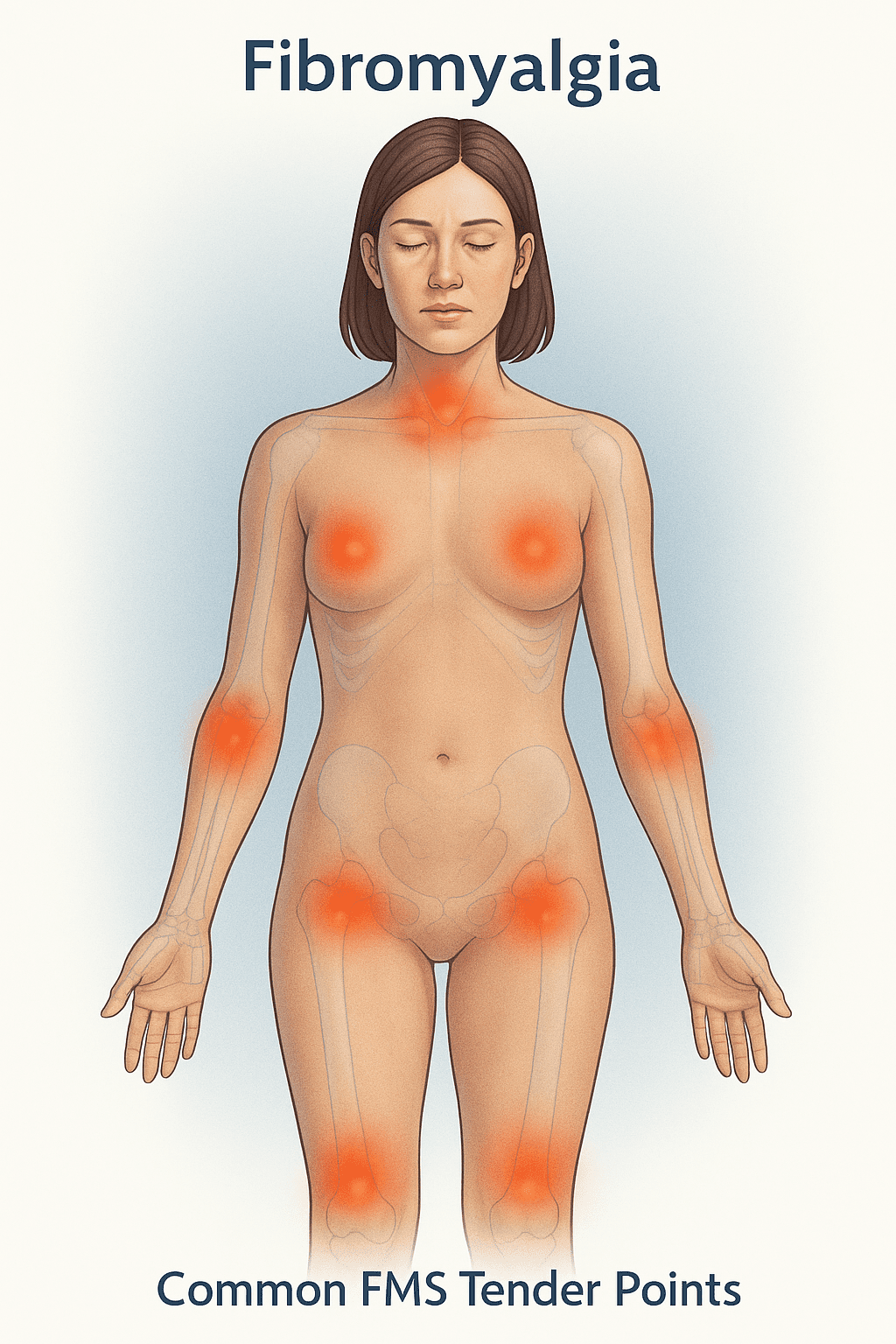
Fibromyalgia (FM) is a modern diagnostic term used to describe a constellation of symptoms—most notably, widespread muscular pain and heightened sensitivity at specific tender points throughout the body. While pain may begin in a localized area such as the neck or shoulders, over time it typically spreads and becomes more generalized.
🧠 Common Symptoms
FM pain is often described as:
- Burning, radiating, gnawing, sore, stiff, or aching
- Fluctuating based on weather, activity, sleep, and stress
- Accompanied by fatigue, often severe, affecting daily function
Many patients describe feeling “flu-like”, even in the absence of an actual infection. Up to 90% of FM patients report profound fatigue, decreased stamina, and unrefreshing sleep.
😴 The Sleep Connection
Sleep studies have shown that many individuals with FM experience abnormal sleep architecture, especially disturbances in deep (restorative) sleep. This may help explain why patients wake feeling exhausted despite a full night’s rest.
🧩 Cognitive & Mood Symptoms
FM often overlaps with Chronic Fatigue Syndrome (CFS). Common overlapping symptoms include:
- Poor memory
- Brain fog
- Difficulty concentrating
- Mood swings
- Confusion
These cognitive and emotional symptoms contribute to the overwhelming nature of FM and its impact on quality of life.
Exploring Root Causes
At its core, FM appears to be part of a broader infection-like or environmental illness syndrome. Triggers may include:
- Undetected bacterial or viral infections
- Environmental toxicants
- Chronic stress and immune dysfunction
In many cases, genetics play a role, influencing how a person responds to a given pathogen or environmental exposure. This helps explain the high variability of symptoms from person to person.
Why Identification Matters
Effective treatment starts with identifying underlying causes. Proper testing can help reveal:
- Hidden infections (bacterial, viral, fungal, or parasitic)
- Immune system imbalances
- Nutritional or mitochondrial deficiencies
- Environmental or toxic burdens
Once the root cause(s) are identified, a targeted treatment plan using nutrition, herbal medicine, lifestyle changes, and in some cases, antimicrobial therapies can support the healing process and improve function.