The Use of Red Light Therapy for Lyme Disease in Healing Tick-Borne Diseases and Mycotoxin Illness
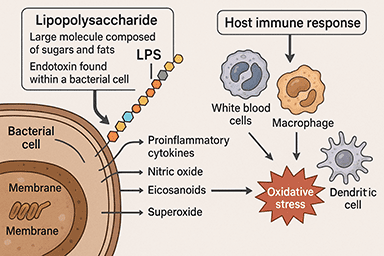
Chronic illnesses like tick-borne diseases, including Lyme disease, Bartonella, and Babesia, as well as mycotoxin-related illness from mold exposure, are notoriously difficult to treat. These conditions often trigger systemic inflammation, oxidative stress, immune dysregulation, and mitochondrial dysfunction — leaving patients feeling exhausted, in pain, and with a range of debilitating symptoms. At Dr. Marra’s integrative medical clinic, we focus on root-cause healing strategies tailored to complex chronic illness.
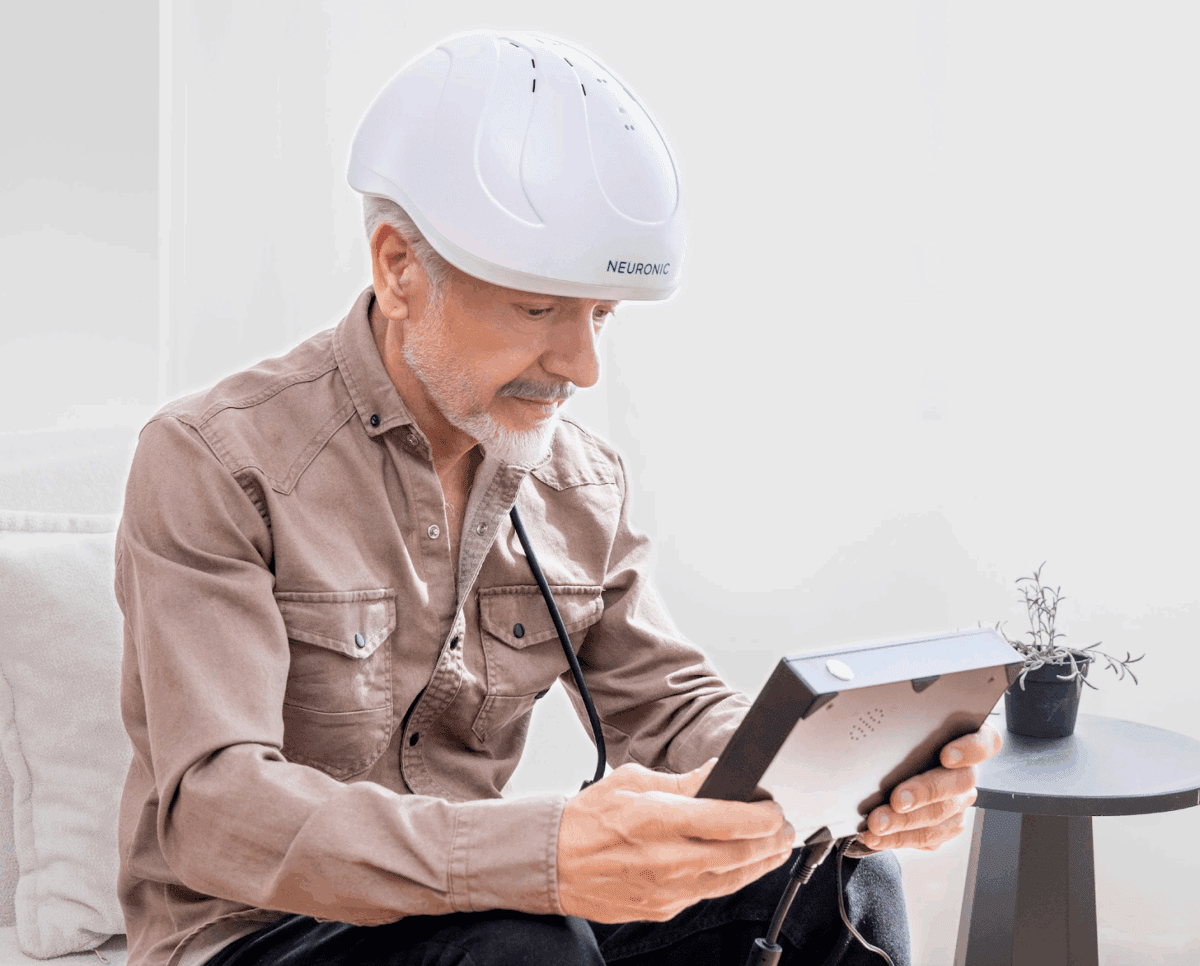
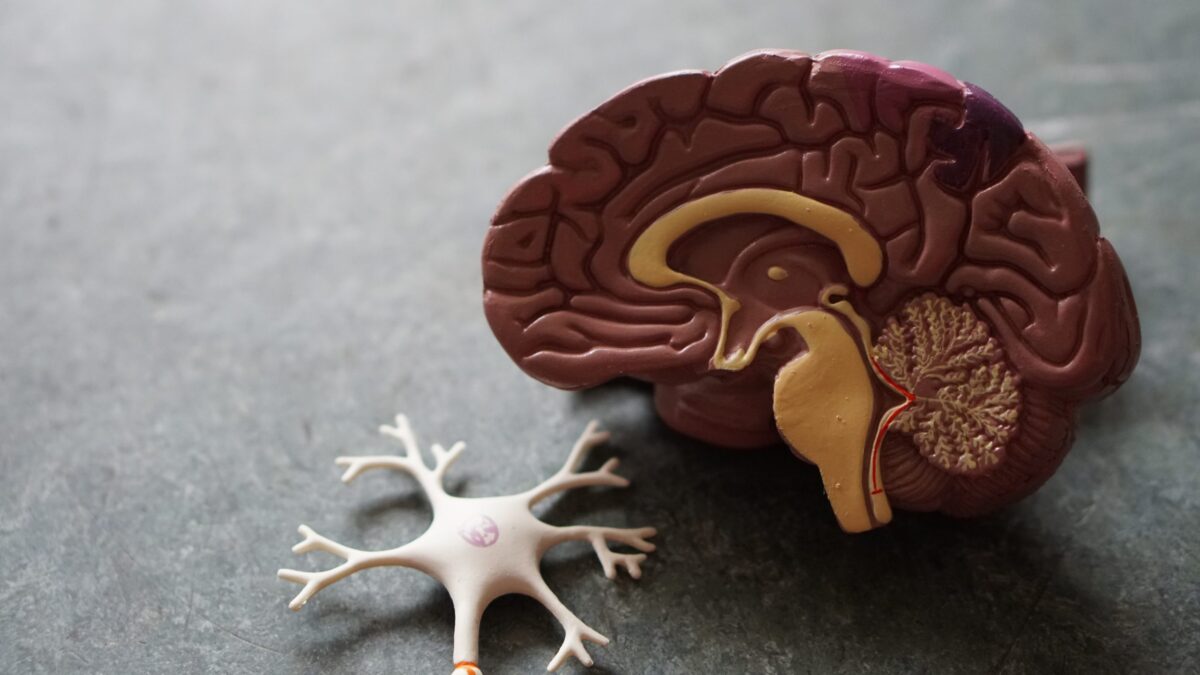
One powerful, science-backed therapy growing in popularity for these conditions is red light laser therapy for Lyme disease, also known as photobiomodulation (PBM). Originally developed in the 1960s, this non-invasive treatment utilizes specific wavelengths of light to support cellular healing.
What Is Red Light Laser Therapy?
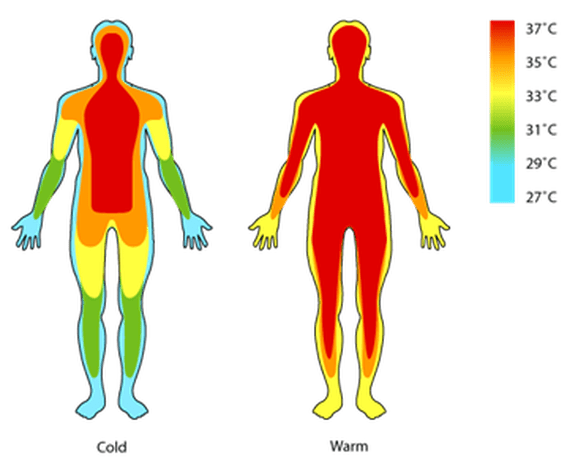
Red light therapy utilizes low-level light wavelengths to penetrate the skin and underlying tissues. Depending on the wavelength, the light can reach different depths in the body:
- Blue light (400–500nm) – targets the skin’s surface, helpful for skin conditions
- Red and near-infrared light (700–1,400nm) – penetrates deeper into soft tissues and organs
- Far-infrared light (3,000–1,000,000nm) – reaches deeper structures, including muscles, bones, and internal organs
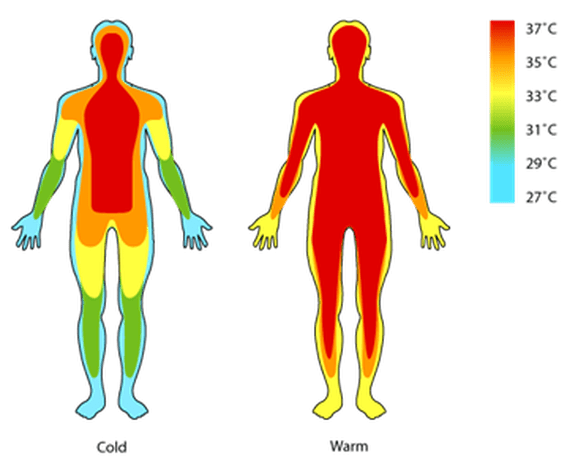
When light is absorbed by cells, it stimulates a molecule in the mitochondria called cytochrome C oxidase, which enhances the conversion of ADP to ATP, your body’s primary source of energy. This boost in ATP production, along with improved blood flow, oxygenation, and nitric oxide release, creates an ideal internal environment for healing.
How Red Light Therapy Helps with Tick-Borne and Mycotoxin Illness
Patients with tick-borne or mold-related illnesses often deal with:
- Mitochondrial dysfunction and low ATP
- Hypoxia (low oxygen in tissues)
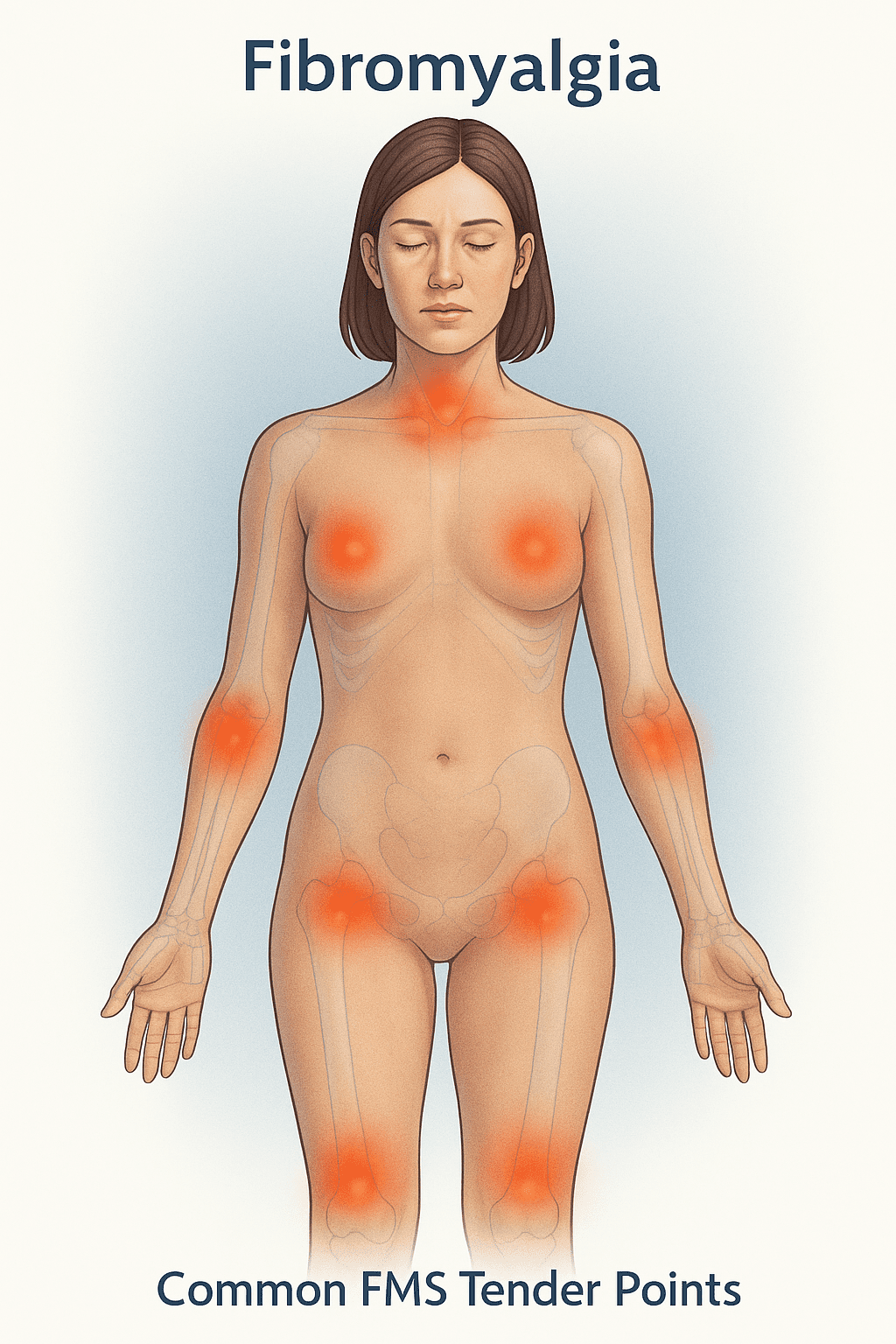
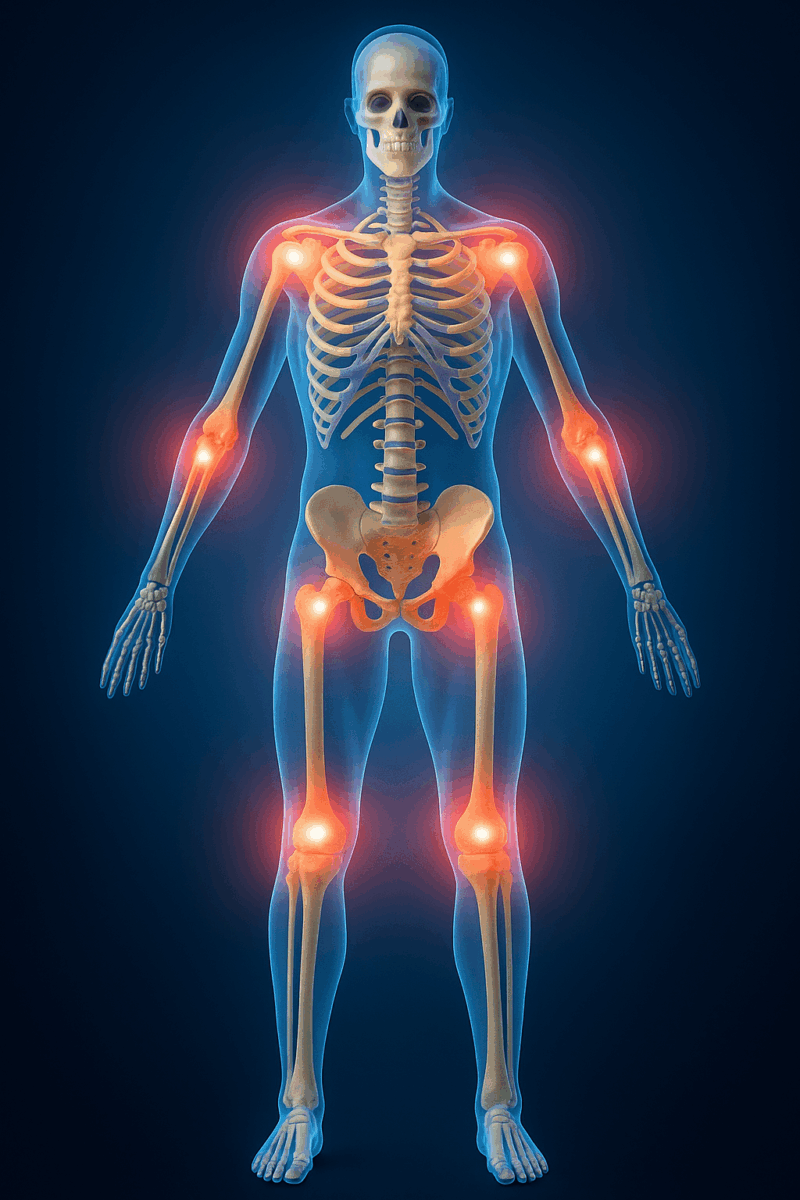
- Chronic pain and neuropathy
- Brain fog and cognitive issues
- Immune dysregulation
- Persistent inflammation
Red light laser therapy directly addresses many of these root causes.
- Reduces Systemic Inflammation: Red light reduces inflammatory cytokines and oxidative stress, allowing the immune system to function more efficiently.
- Boosts Mitochondrial Energy Production: In conditions like Bartonella, where VEGF and HIF pathways are disrupted, PBM helps normalize oxygen sensing and ATP generation at the cellular level.
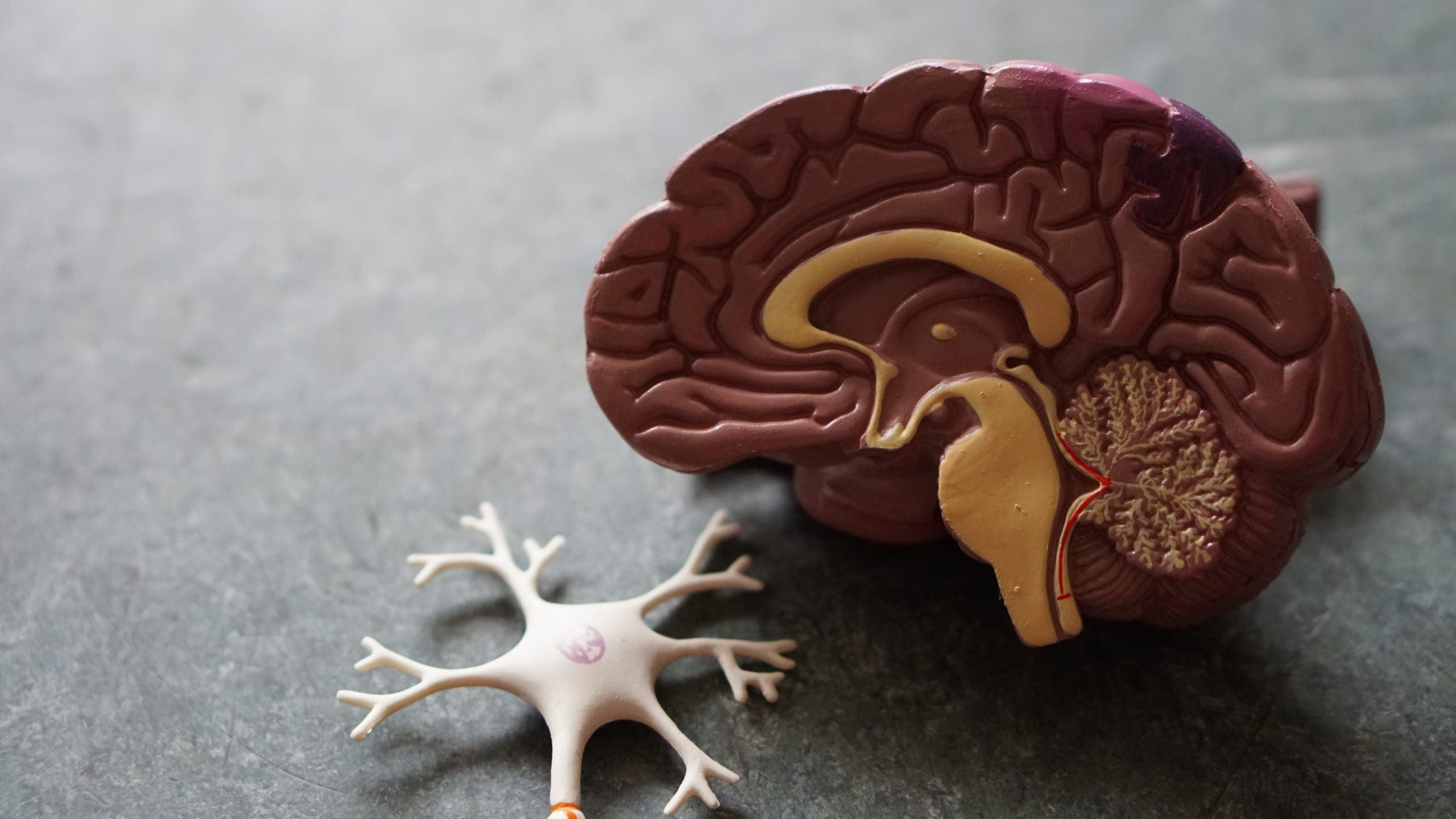
- Enhances Brain Function: Infrared light penetrates deep into the brain, improving blood flow, neural connectivity, and cognitive performance. Patients with neurological symptoms, common in Lyme and mold illness, often report improved clarity, memory, and mood.
- Improves Circulation and Tissue Repair: By stimulating the release of nitric oxide and enhancing oxygen delivery, red light therapy promotes the healing of damaged tissues, nerves, and organs affected by chronic infections or toxic mold exposure.
Conditions Treated with Red Light Laser Therapy
In Dr. Marra’s office, we use red light laser therapy to help with a wide range of conditions, including:
- Inflammation & Pain Relief
- Neuropathy (burning, stinging, numbness)
- Cognitive dysfunction (brain fog, fatigue)
- Sleep disorders & circadian rhythm imbalance
- Mood disorders like depression and anxiety
- Chronic joint and muscle pain
- Immune system support
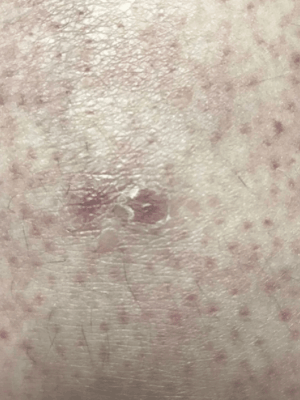
- Wound healing and skin repair
- Gut dysbiosis and esophageal injury
- Fatigue, tremors, and overall energy restoration
For patients with tick-borne diseases and mycotoxin illnesses, these benefits can be life-changing, especially when combined with a comprehensive integrative treatment plan.
Are There Any Contraindications?
While red light therapy is safe for most people, it is not recommended for patients with:
- Seizure disorders
- Light hypersensitivity
- Active cancer
- Pregnancy
- Open, oozing skin lesions
Dr. Marra will review your medical history to ensure it’s the right fit for you.
Book a Red Light Therapy for Lyme Disease Session with Dr. Marra
If you’re struggling with the long-term effects of Lyme disease, tick-borne infection, or mycotoxin exposure, red light therapy for Lyme disease may be a powerful tool in your recovery.
To schedule a session or learn more about photobiomodulation therapy, contact Dr. Marra’s office online or call 206-299-2676. We offer package deals to help make your healing journey affordable, accessible, and impactful.
More Resources:
- How a Red Light Therapy Helmet Can Boost Brain Health and Mood
- Revolutionize Your Healing with Firefly Red Light Laser Technology
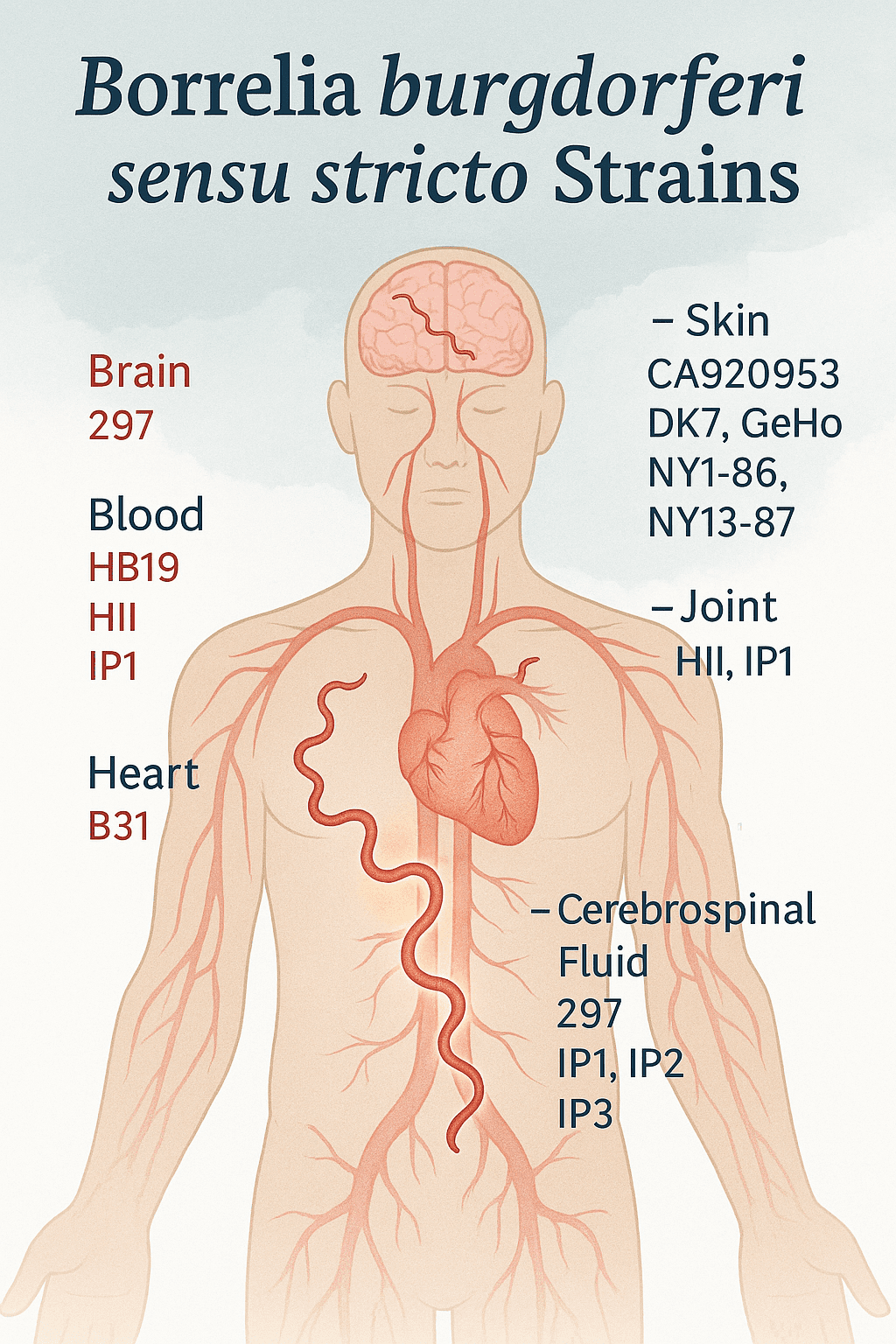
- Borrelia burgdorferi Strains
- Patient Resources: Recommendations for Patients Infected with Tick-Borne Illness
Disclaimer: This article is for informational purposes only. It is not a substitute for medical advice. Always consult your healthcare provider for diagnosis or treatment.