Babesiosis
Babesiosis, often a co-infection of Lyme Disease in humans, was first identified by Victor Babes in the late 19th century in Romanian cattle and the disease at that time was coined “Red Water Fever.” However, Babesia infection in humans was not confirmed until 1956 in a Yugoslavian farmer.
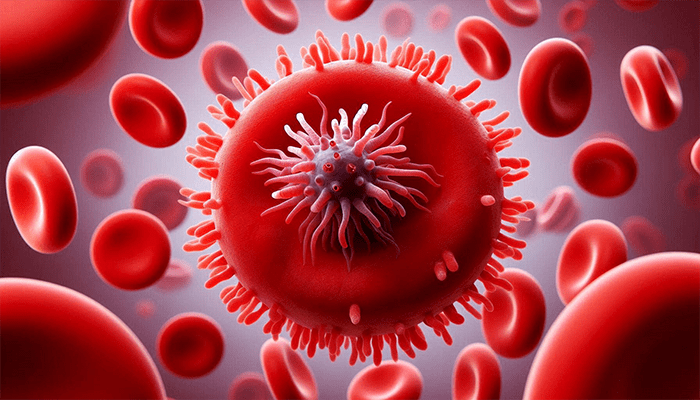
Babesia is a protozoan intracellular red blood cell parasite quite similar to malaria and is a worldwide emerging zoonotic disease. There are about 100 known species of Babesia that infect livestock animals and rodents. However, the three currently known species causing human disease, B. microtii, and B. duncani (formerly WA1 and first identified in Washington state but found throughout the United States), and Babesia divergens (found in Europe), are largely found in the northern hemisphere. The islands of Nantucket and Martha’s Vineyard on the eastern coast of Massachusetts, are considered endemic for Babesia species, however, migratory birds are likely to transport vectors of all tick-borne illnesses, which may account for the bacteria’s presence on the west coast as well. Currently, scientists believe that there may be additional human pathogenic species such as B. bigemina and B. bovisbut further researcher is necessary for this area of infectious disease.
Babesia infection is transmitted through a tick bite or contaminated blood products, where sporozoites directly enter the bloodstream and infect red blood cells that contain a heme structure, where an iron molecule resides for oxygen binding purposes. Babesia interferes with red blood cell function, giving rise to common symptoms of night sweats, air hunger, shortness of breath, severe headaches, and often anemia of chronic disease. Serologically, low hemoglobin, hematocrit, and/or red blood cell count, as well as low ferritin and transferrin, may accompany this disease. Additionally, there are two confirmed human cases of maternal transplacental transmission in humans.
Laboratory testing for Babesia species can be difficult and serum antibodies, as well as fluorescent in situ hybridization techniques and PCR (polymerase chain reaction) tests, maximize the chances of documenting the presence of this bacteria. Additionally, infected hosts may have subclinical parasitemia which yields greater difficulty in laboratory detection. Babesia can also be observed in a Giemsa stain where the organism appears like a “Maltese cross.”
Since Babesia species are parasites, antiparasitic herbs and pharmacology are required to treat fulminant disease. The presence of this bacteria in an already infected Lyme patient or an immunocompromised or splenectomized (spleen removal) patient, can complicate treatment substantially. However, antimalarial medications are typically used and shed light on a wider variety of treatment choices for this infection, especially when coupled with Lyme Disease.
The last 20 years have been marked by the global proliferation of human Babesia infections, and suspicion for this disease should be considered whenever a tick bite has been noted, even if a Bullseye rash is not noted at the site of the bite. Babesia infection may be transmitted with or without Lyme Disease and it is not known to be associated with a Bullseye rash.
Contact our office for more information regarding this global emerging zoonotic disease for proper diagnosis treatment.
